Background:
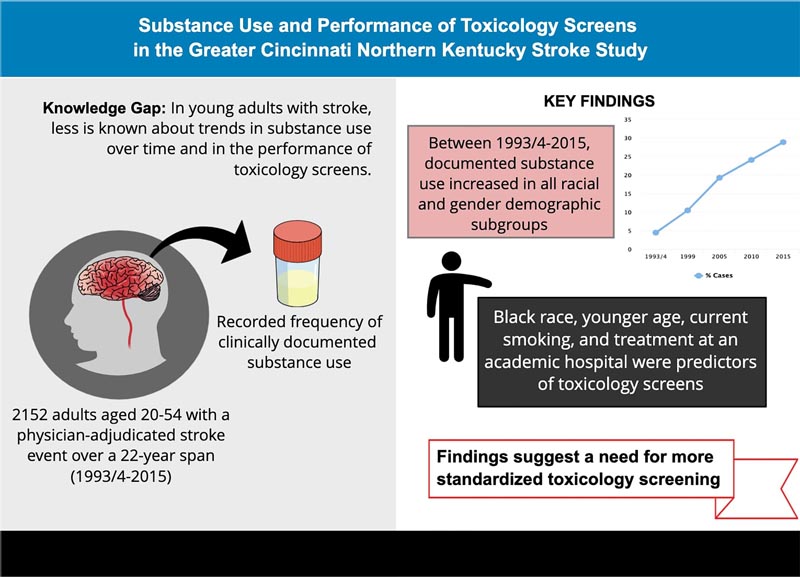
Although risk factors for stroke, such as substance use, may vary with age, less is known about trends in substance use over time or the performance of toxicology testing in young adults with stroke. stroke.
Methods:
Using the Northern Kentucky Greater Cincinnati Stroke Study, a population-based study in a 5-county region comprising 1.3 million people, we report the frequency of documented substance use (cocaine/marijuana/ opiates/other ). obtained from review of electronic medical records, overall and by race/gender subgroups among physician-adjudicated strokes (ischemic and hemorrhagic) in adults 20 to 54 years of age.
Secondary analyzes included excessive alcohol consumption and smoking . Data were reported for 5 one-year periods spanning 22 years (1993/1994–2015), and trends over time were tested. For 2015, to evaluate factors associated with toxicology testing performance, multiple logistic regression was performed.
Results
In total, 2,152 strokes were included: 74.5% were ischemic , the mean age was 45.7 ± 7.6, 50.0% were women and 35.9% were black.
Substance use was documented in 4.4%, 10.4%, 19.2%, 24.0%, and 28.8% of cases in 1993/1994, 1999, 2005, 2010, and 2015, respectively ( Ptrend<0.001). Between 1993/1994 and 2015, documented substance use increased across all demographic subgroups.
When adjusting for sex, comorbidities, and the National Institutes of Health Stroke Scale, predictors of toxicology screening included black race (adjusted odds ratio, 1.58 [95% CI, 1.02–2.45]). , younger age (adjusted odds ratio, 0.70 [95% CI, 0.53–0.91], by 10 years), current smoking (adjusted odds ratio, 1.62 [95% CI, 1.06–0.91], 2.46]) and treatment at an academic hospital (adjusted odds ratio, 1.80 [95% CI, 1.14–2.84]).
Conclusions:
In a population-based study of young adults with stroke, documented substance use increased over time, and documentation of substance use was higher among blacks compared to whites.
More work is needed to confirm race-based disparities and trends in substance use given the potential for bias in detection and documentation. The findings suggest the need for more standardized toxicological evaluation.
Comments
Documented cocaine and marijuana use among young adults who have suffered strokes has increased substantially in recent decades, especially among white men and women, new research suggests.
Overall, however, documented substance use among stroke patients was highest among young black men. The authors of the study, published Thursday in the American Heart Association’s journal Stroke , suggested that bias in who gets a drug test after a stroke may be skewing the data, and they recommend developing more standardized guidelines. for the toxicological evaluation of patients with stroke.
"We don’t know if it’s due to a bias in who is tested or if there are real differences in substance use," said Dr. Tracy Madsen, one of the lead authors. Madsen is an associate professor of emergency medicine and epidemiology at the Alpert School of Medicine of Brown University in Providence, Rhode Island.
"This is important because we are seeing the incidence of stroke in young adults increase over time ," he said. Although the study did not look at whether marijuana, cocaine or other substance use was causing the increase in strokes among young adults, Madsen suggested the trend be explored further given the high rate of death and disability associated with having a stroke. in young adults. years.
About 10% of all strokes in the U.S. occur among adults age 50 and younger , whose mortality rate is four times that of the general population. Disability caused by a stroke can deprive young adults of their most productive years.
Previous research has shown an increase in strokes in younger adults, as well as an increase in substance use among this age group. While traditional stroke risk factors, including high blood pressure, diabetes, high cholesterol, and obesity, contribute to stroke risk for young adults, they may not account for all of the increase.
"It’s really quite urgent to figure out what kind of risk factors we see in this age group, so we can do a better job of preventing stroke," Madsen said.
Using data from the Greater Cincinnati Northern Kentucky Stroke Study, which covers five counties in southern Ohio and northern Kentucky, researchers analyzed the use of cocaine, marijuana, opioids and "other" drugs among 2,152 adults ages 20 to 20. 54 years old who suffered strokes. They also looked at heavy drinking and smoking over a 22-year period.
From 1993 to 2015, documented drug use, especially marijuana and cocaine use, increased among all groups in the study, but appears to have increased the most among white men and women. Among black adults who suffered strokes, it increased from 1993 to 2005 and then remained stable. Overall, heavy drinking and smoking remained stable over the two-decade study period, although heavy drinking declined among black men.
Black adults who had a stroke were 58% more likely to be screened for substance use than white adults. Age also made a difference. For every 10 years, older people were 30% less likely to have a toxicology test.
Where a person was treated for stroke made an even bigger difference. Those treated at academic stroke centers were 80% more likely to receive a drug test than those treated at community hospitals. "Academic centers may have established protocols for conducting toxicology screenings," Madsen said.
Without standardized protocols for toxicology evaluation after stroke, it is difficult to know what role substance use may play and among which groups, Madsen said.
Additionally, more research is needed to understand how a positive drug test affects the treatment stroke patients receive, he said. "Is it for better or worse? Are they getting all the tests they need, or do doctors assume they had a stroke because of their substance use? The answers to these questions would help decide whether we say that all patients with stroke should be examined."
Dr. Steven Kittner, a professor of neurology at the University of Maryland School of Medicine in Baltimore, who was not involved in the research, said this needs to be looked at more closely.
A toxicology test "is not a substitute for a thorough evaluation" of the cause of a person’s stroke, he said.
"As long as that’s emphasized, there’s really no downside to screening for drug use in this early-onset stroke population."
Kittner noted that the study did not include a control group of people who did not have strokes, so no conclusions can be drawn about whether substance use is causing strokes among young adults. "That wasn’t really her focus."
Cocaine use has been linked to an increased risk of stroke in previous studies, Madsen said. "But we know much less about whether marijuana leads to an increased risk of stroke." Given the rise in marijuana legalization, he said, "this should be explored."
One option is to evaluate only stroke patients in whom no other potential cause of the stroke can be identified, Madsen said. It is also important that those who test positive for substance use receive counseling and treatment, a recommendation supported by the 2021 AHA guidelines for stroke prevention.
















