Background
Casirivimab and imdevimab are non-competitive monoclonal antibodies that bind to two different sites on the receptor-binding domain of the SARS-CoV-2 spike glycoprotein, blocking viral entry into host cells.
Our objective was to evaluate the efficacy and safety of casirivimab and imdevimab administered in combination in hospitalized patients with COVID-19.
Methods
RCOVERY is an open-platform, controlled, randomized trial comparing several potential treatments with usual care in hospitalized patients with COVID-19.
127 UK hospitals participated in the evaluation of casirivimab and imdevimab. Eligible participants were any patient at least 12 years old admitted to hospital with clinically suspected or laboratory-confirmed SARS-CoV-2 infection.
Participants were randomly assigned (1:1) to standard-of-care alone or to standard-of-care plus casirivimab 4 g and imdevimab 4 g administered together as a single intravenous infusion. Investigators and data evaluators were blinded to analyzes of outcome data during the trial.
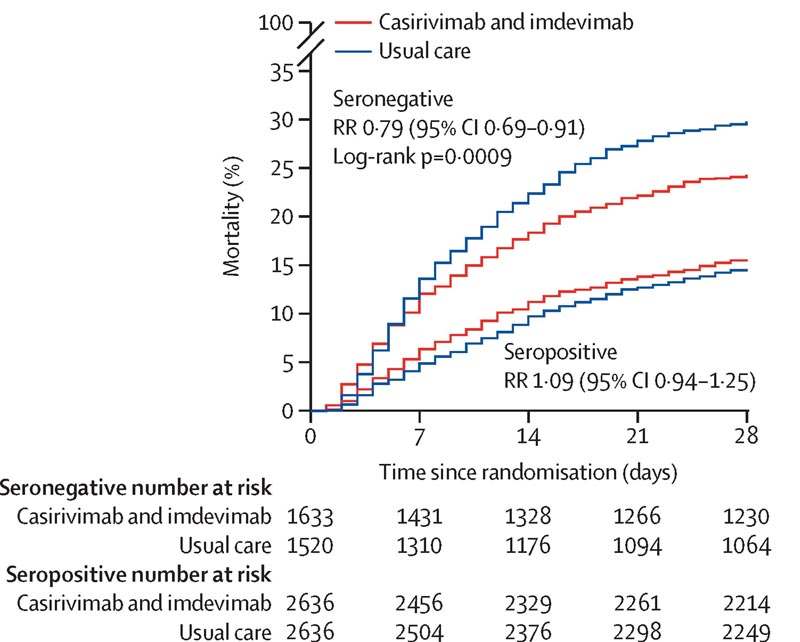
The primary outcome was 28-day all-cause mortality assessed on an intention-to-treat basis, first only in patients without detectable antibodies to SARS-CoV-2 infection at randomization (i.e., those who were seronegative) and then in the general population.
Safety was assessed in all participants receiving casirivimab and imdevimab.
The trial is registered with ISRCTN (50189673) and ClinicalTrials.gov (NCT04381936).
Results
Between September 18, 2020 and May 22, 2021, 9,785 patients enrolled in RECOVERY were eligible for casirivimab and imdevimab, of whom 4,839 were randomly assigned to casirivimab and imdevimab plus usual care and 4,946 to usual care alone. 3153 (32%) of 9785 patients were seronegative, 5272 (54%) were seropositive, and 1360 (14%) had unknown baseline antibody status.
812 (8%) patients were known to have received at least one dose of a SARS-CoV-2 vaccine. In the primary efficacy population of seronegative patients, 396 (24%) of 1633 patients assigned to casirivimab and imdevimab versus 452 (30%) of 1520 patients assigned to usual care died within 28 days (rate ratio [RR] 0 79.95% CI 0 69–0 91; p=0 0009).
In an analysis of all randomized patients (regardless of baseline antibody status), 943 (19%) of 4839 patients assigned to casirivimab and imdevimab versus 1029 (21%) of 4946 patients assigned to usual care died within 28 days (RR 0·94, 95% CI 0.86-1.02, p=0.14).
The proportional effect of casirivimab and imdevimab on mortality differed significantly between HIV-positive and HIV-negative patients (p value for heterogeneity = 0.002).
There were no deaths attributed to treatment, and no significant differences between groups in the prespecified safety outcomes of cause-specific mortality, cardiac arrhythmia, thrombosis, or major bleeding events.
Serious adverse reactions reported in seven (<1%) participants were considered by the local investigator to be related to treatment with casirivimab and imdevimab.
Monoclonal neutralizing antibodies are effective in hospitalized COVID-19 patients who have not developed their own antibody response ("seronegative"), but not in those who have ("seropositive"). Casirivimab + imdevimab (from Regeneron)
|
Interpretation
In patients admitted to the hospital with COVID-19, the monoclonal antibody combination of casirivimab and imdevimab reduced 28-day mortality in patients who were seronegative (and therefore had not mounted their own humoral immune response) at baseline, but not in those who were seropositive at baseline. base.
UK Research and Innovation (Medical Research Council) and National Institute for Health Research.