Blood pressure reduction and risk of new-onset type 2 diabetes: a meta-analysis of individual participant data
Highlights It is well established that blood pressure control is an important strategy to reduce cardiovascular events among people with diabetes. But can lowering blood pressure reduce the risk of developing type 2 diabetes in the first place? And, if so, does the medication we prescribe to achieve this goal make a difference? This data analysis, which included studies with more than 145,000 participants, reveals that a 5 mm Hg reduction in systolic blood pressure was associated with an 11% reduction in the risk of developing type 2 diabetes. Among the major antihypertensive drug classes, ACE inhibitors and ARBs were associated with a lower risk of developing diabetes, calcium channel blockers did not have a statistically significant impact, but beta blockers and thiazide diuretics increased the risk of developing diabetes. . This study has important implications for diabetes prevention strategies in primary care settings, as well as for the treatments we choose to control hypertension. |
Background
Lowering blood pressure is an established strategy to prevent the micro- and macrovascular complications of diabetes, but its role in preventing diabetes itself is unclear.
The aim of this study was to examine this question using individual participant data from major randomized controlled trials.
Methods
A single-stage individual participant data meta-analysis was performed, in which data were pooled to investigate the effect of blood pressure lowering per se on the risk of new-onset type 2 diabetes.
Network meta-analysis of individual participant data was used to investigate the differential effects of five major classes of antihypertensive drugs on the risk of new-onset type 2 diabetes.
Overall, data from 22 studies conducted between 1973 and 2008 were obtained by the Blood Pressure Lowering Treatment Trialists’ Collaboration (University of Oxford, Oxford, United Kingdom). We included all primary and secondary prevention trials that used a specific class or classes of antihypertensive drugs versus placebo or other classes of hypotensive drugs that had at least 1000 person-years of follow-up in each randomized arm.
Participants with a known diagnosis of diabetes at baseline and trials conducted in patients with prevalent diabetes were excluded . The stratified Cox proportional hazards model was used for single-stage meta-analysis of individual participant data, and logistic regression models were used for network meta-analysis of individual participant data to calculate the relative risk (RR) for comparisons of classes of drugs.
Results
145,939 participants (88,500 [60-6%] men and 57,429 [39-4%] women) from 19 randomized controlled trials were included in the one-stage individual participant data meta-analysis.
Twenty-two trials were included in the network meta-analysis of data from individual participants. After a median follow-up of 4-5 years (IQR 2-0), 9883 participants were diagnosed with new-onset type 2 diabetes.
Reducing systolic blood pressure by 5 mm Hg reduced the risk of type 2 diabetes in all trials by 11% (hazard ratio 0-89 [95% CI: 0-84-0-95]).
Investigation of the effects of five major classes of antihypertensive drugs showed that, compared with placebo, angiotensin-converting enzyme inhibitors (RR 0-84 [95% 0-76-0-93]) and blockers of angiotensin II receptors (RR 0-84 [0-76-0-92]) reduced the risk of new-onset type 2 diabetes; However, the use of β-blockers (RR 1-48 [1-27-1-72]) and thiazide diuretics (RR 1-20 [1-07-1-35]) increased this risk, and was not found no material effect for calcium channel blockers (RR 1-02 [0-92-1-13]).
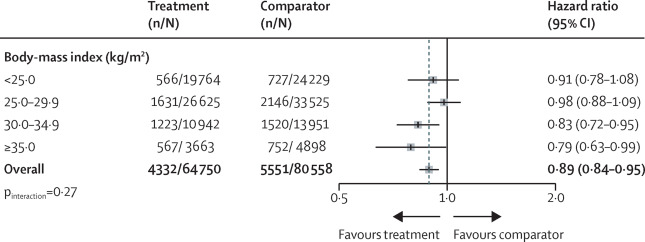
Blood pressure-lowering treatment and risk of new-onset type 2 diabetes, by baseline body mass index categories
Interpretation
However, established pharmacological interventions have qualitatively and quantitatively different effects on diabetes, probably due to their different off-target effects, with angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers having the most favorable results. This evidence supports the indication of certain classes of antihypertensive drugs for diabetes prevention, which could further refine drug selection based on an individual’s clinical risk for diabetes. |
Possible mechanisms
Although the exact biological pathways through which elevated blood pressure causes new-onset type 2 diabetes are unknown, several potential mechanisms have been described. Among others, insulin resistance, vascular inflammation and endothelial dysfunction , which usually precede the clinical manifestation of diabetes, are pathophysiological consequences of hypertension.
Insulin resistance could play a critical role in the interplay between metabolism and cardiovascular pathways.
Other pathways, such as increased activation of the sympathetic nervous system and chronic inflammation leading to endothelial dysfunction, have also been suggested as links between hypertension and diabetes risk.
It should be noted that the effect of antihypertensive drug classes on these mediating factors is variable and could explain their different off-target effects. For example, renin-angiotensin inhibition has been shown to reduce the concentration of inflammatory markers, independently of the blood pressure-lowering effect, which could enhance its protective effect on diabetes.
Another plausible biological mechanism for its protective effect is the improvement of insulin resistance by suppressing reactive oxygen species.
In the case of β-blockers and thiazide diuretics, although the biological pathway of diabetes risk is not known with certainty, studies have suggested that the modification of insulin secretion and carbohydrate metabolism in β-blockers and potassium depletion in thiazide diuretics could play a role. Furthermore, CCBs have no known material effects on these mediating mechanisms or could have additional pathophysiological sequelae that negate their blood pressure-lowering effect.
More experimental studies are needed to explore these and other possible mechanisms. Furthermore, by demonstrating that diabetes risk can be modified with drugs that do not target hyperglycemia, this study encourages future research to identify other molecular targets for diabetes prevention.
Implications of all available evidence
This study suggests that lowering blood pressure may help prevent diabetes, in addition to its well-established beneficial effects in reducing cardiovascular events.
The relative magnitude of the reduction per 5 mm Hg decrease in systolic blood pressure was similar to those reported for the prevention of major cardiovascular events, which will strengthen the case for blood pressure reduction through interventions such as of life that are known to lower blood pressure, and blood pressure lowering treatments with drugs, and possibly device therapies.
The different effects of some classes of drugs also support decision-making for the choice of drugs according to the risk profile of each individual. In particular, angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists should be the drugs of choice when the clinical risk of diabetes is a concern, while β-blockers and thiazide diuretics They should be avoided whenever possible.
This study also encourages further research to identify and clinically test alternative mechanisms for diabetes prevention that do not necessarily target hyperglycemia. Thus, this research could provide additional avenues to curb the growing burden of diabetes.
















