Key points Which COVID-19 patients can benefit from prolonged thromboprophylaxis after hospital discharge? Findings In this cohort study of 2832 hospitalized patients with COVID-19, post-discharge venous thromboembolic events occurred more frequently in those with a history of venous thromboembolism, maximum dimerized plasmin D fragment (D-dimer) level greater than 3 μg/ ml and before discharge C-reactive protein level greater than 10 mg/dL. Patients who received anticoagulation therapy after discharge had fewer events. Meaning These findings suggest that post-discharge anticoagulation therapy may be considered for high-risk patients with COVID-19. |
COVID-19 induces coagulopathy that manifests as elevated levels of the dimerized plasmin D fragment (D-dimer). As a result, patients with COVID-19 frequently experience both arterial thromboembolism (ATE) and venous thromboembolism (VTE). Bourguignon et al reported that pulmonary embolism and deep vein thrombosis occurred in 20.6% to 49.0% of COVID-19 patients treated in intensive care units (ICUs).
In many facilities, high-risk patients with COVID-19 receive anticoagulation (AC) at doses higher than the prophylactic dose for primary VTE prophylaxis during their hospitalization.
AC treatment in hospitalized patients with COVID-19 is associated with reduced mortality.
Of note, the risk of ASD and VTE in patients with COVID-19 extends beyond their hospitalization.
These thrombotic events are associated with readmission and mortality 90 days after discharge from the index admission. To mitigate the risk of VTE, a short-term course of AC has been used in patients with COVID-19 after hospital discharge. However, this practice is challenged by the low incidence of VTE in unselected patients with COVID-19.
Giannis et al. reported that 1.55% of COVID-19 patients experienced VTE within 90 days of discharge. Universal prescribing of AC after discharge in patients with COVID-19 offers marginal clinical benefits and may cause harm in patients at high risk of bleeding. Given the unclear evidence, clinicians face the dilemma of which hospitalized patients with COVID-19 might benefit from post-discharge CA.
We conducted a cohort study of COVID-19 patients discharged from a hospital stay to evaluate the rate of post-discharge thrombosis in patients with COVID-19, identify factors associated with the risk of post-discharge VTE, and evaluate the association of AC use post-discharge. with incidence of VTE.
Importance
COVID-19 is associated with a high incidence of thrombotic events; however, the need for prolonged thromboprophylaxis after hospitalization remains unclear.
Aim
To quantify the rate of arterial and venous thromboembolism after discharge in patients with COVID-19, identify factors associated with the risk of venous thromboembolism after discharge, and evaluate the association of anticoagulant use after discharge with the incidence of venous thromboembolism.
Design, environment and participants
This is a cohort study of adult patients hospitalized with COVID-19 confirmed by a positive SARS-CoV-2 test. Eligible patients were enrolled at 5 Henry Ford Health System hospitals from March 1 to November 30, 2020. Data analysis was conducted from April to June 2021.
Exhibitions
Anticoagulant therapy after discharge.
Main results and measures
New onset of symptomatic arterial and venous thromboembolic events within 90 days of discharge from initial admission for COVID-19 infection were identified using codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision.
Results
In this cohort study of 2,832 adult patients hospitalized with COVID-19, the mean (SD) age was 63.4 (16.7) years (IQR, 53-75 years) and 1,347 patients (47.6%) were men. Thirty-six patients (1.3%) presented venous thromboembolic episodes after discharge (16 pulmonary embolism, 18 deep vein thrombosis and 2 portal vein thrombosis).
Fifteen (0.5%) post-discharge arterial thromboembolic events were observed (1 transient ischemic attack and 14 acute coronary syndrome).
The risk of venous thromboembolism decreased over time (Mann-Kendall trend test, p < 0.001), with a median (IQR) time to event of 16 (7-43) days.
There was no change in the risk of arterial thromboembolism over time (Mann-Kendall trend test, P = .37), with a median (IQR) time to event of 37 (10-63) days.
Patients with a history of venous thromboembolism (odds ratio [OR], 3.24; 95% CI, 1.34-7.86), maximum level of dimerized plasmin D fragment (D-dimer) greater than 3 μg/ml ( OR, 3.76; 95% CI, 1.86-7.57), and a pre-discharge C-reactive protein level greater than 10 mg/dL (OR, 3.02; 95% CI, 1. 45-6.29) were more likely to experience venous thromboembolism after discharge.
Therapeutic anticoagulation prescriptions at discharge were associated with a lower incidence of venous thromboembolism (OR, 0.18; 95% CI, 0.04-0.75; p = 0.02).
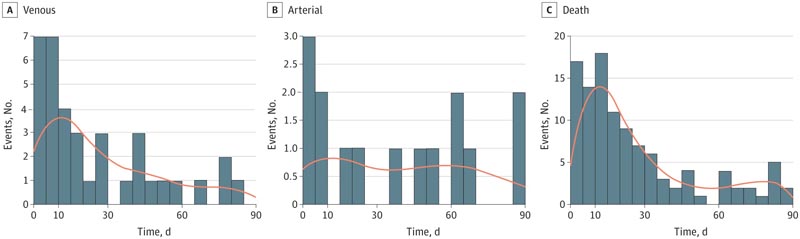
Count of post-discharge venous thromboembolism events, arterial thromboembolism, and death without events
Discussion
We conducted a cohort study involving 2,832 adult patients hospitalized with COVID-19 to address the controversy over AC use after discharge. Our study has reiterated the low incidence of symptomatic VTE in COVID-19 patients after discharge, which was comparable to other studies. To our knowledge, this study is the first so far that has captured sufficient post-discharge VTE events to be able to identify factors associated with increased risk.
We demonstrated that hospitalized COVID-19 patients who had a history of VTE, a pre-discharge CRP level greater than 10 mg/ml, or a peak D-dimer level during hospitalization greater than 3 μg/ml were predisposed to experience a new occurrence of VTE after discharge.
Patients with these characteristics were considered a high-risk population.
Post-discharge therapeutic CA was associated with a reduced risk of VTE in all COVID-19 patients requiring hospitalization. Because high-risk patients with COVID-19 had a higher incidence of VTE after discharge compared to other subpopulations, post-discharge therapeutic AC may benefit them more. Our findings may help inform future post-discharge CA policy for hospitalized patients with COVID-19.
Conclusions and relevance Although prolonged thromboprophylaxis in unselected patients with COVID-19 is not supported, these findings suggest that post-discharge anticoagulation may be considered in high-risk patients who have a history of venous thromboembolism, peak D-dimer level greater than 3 μg/ ml and a pre-discharge C-reactive protein level greater than 10 mg/dL, if your bleeding risk is low. |