The current outbreak of coronavirus disease 2019 (COVID-19) vividly demonstrates the burden respiratory infectious diseases impose on an intimately connected world. Unprecedented mitigation and containment policies have been implemented in an effort to limit the spread of COVID-19, including travel restrictions, screening and testing of travelers, isolation and quarantine, and school closures.
A key goal of such policies is to decrease encounters between infected individuals and susceptible individuals and slow the rate of transmission. Although such social distancing strategies are critical at the current time of the pandemic, it may seem surprising that the current understanding of host-to-host transmission routes in respiratory infectious diseases is based on a model of disease transmission developed in the 1990s. 1930 which, by modern standards, seems oversimplified.
Implementing public health recommendations based on these older models may limit the effectiveness of proposed interventions.
Understanding the transmission of respiratory infectious diseases
In 1897, Carl Flügge demonstrated that pathogens were present in expiratory droplets large enough to settle around an infected individual. “Droplet transmission” by contact with the expelled and infected liquid phase of droplets was thought to be the primary route for respiratory disease transmission. This view prevailed until William F. Wells focused on tuberculosis transmission in the 1930s and dichotomized respiratory droplet emissions into "large" and "small" droplets .
According to Wells, isolated droplets are emitted when exhaling.
- Large droplets settle faster than they evaporate, contaminating the immediate vicinity of the infected individual.
- In contrast, small droplets evaporate faster than they settle.
In this model, as small droplets move from the warm, humid conditions of the respiratory system to the colder, drier outside environment, they evaporate and form residual particles made from the dried material of the original droplets.
These residual particles are called droplet nuclei or aerosols.
These ideas resulted in a dichotomous classification between large versus small droplets, or droplets versus aerosol, which can then mediate the transmission of respiratory diseases. Infection control strategies were developed based on whether a respiratory infectious disease is transmitted primarily via the large or small droplet route.
The dichotomy between large and small droplets remains at the core of the classification systems for respiratory disease transmission routes adopted by the World Health Organization and other agencies, such as the Centers for Disease Control and Prevention. These classification systems employ several arbitrary droplet diameter cutoffs, from 5 to 10 μm, to classify host-to-host transmission as droplets or aerosol pathways.1
Such dichotomies continue under current risk management, key recommendations and resource allocation for response management associated with infection control, including for COVID-19. Even when maximum containment policies were applied, the rapid international spread of COVID-19 suggests that the use of arbitrary droplet size limits may not accurately reflect what is actually happening with respiratory emissions, possibly contributing to the ineffectiveness of some procedures. used to limit the spread of respiratory diseases.
New model for respiratory emissions
Recent work has shown that exhalations, sneezes, and coughs not only consist of mucosal droplets following short-range semiballistic emission trajectories, but are primarily formed by a multiphase turbulent gas cloud (a cloud) that traps ambient air and carries a continuum of droplet sizes.
The locally moist and warm atmosphere within the turbulent gas cloud allows contained droplets to evade evaporation for much longer than isolated droplets do. Under these conditions, the lifetime of a droplet could be significantly extended by a factor of up to 1000, from a fraction of a second to minutes.
Due to the forward momentum of the cloud, pathogen-carrying droplets are propelled much further than if they were emitted in isolation without being caught and carried forward by a cloud of turbulent clouds.
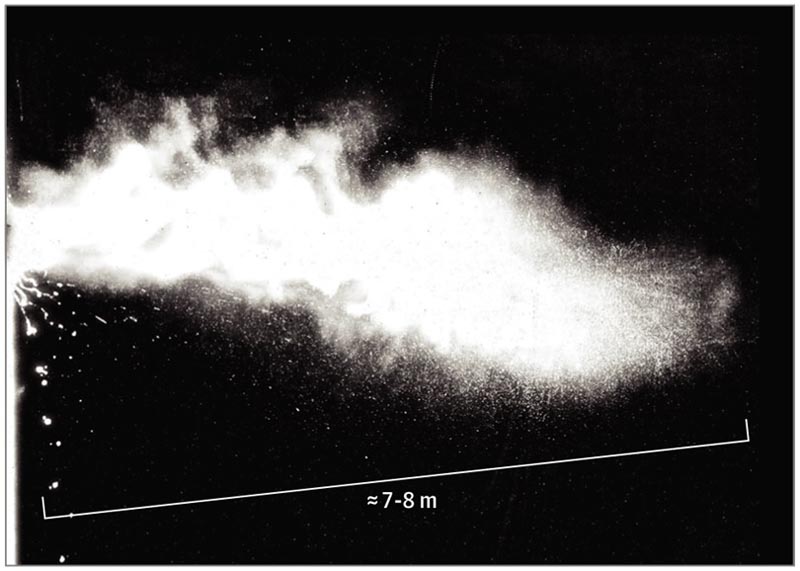 Multiphase turbulent gas cloud from a human sneeze
Multiphase turbulent gas cloud from a human sneeze
Given the various combinations of an individual patient’s physiology and environmental conditions, such as humidity and temperature, the gas cloud and its payload of pathogenic droplets of all sizes can travel 23 to 27 feet ( 7-8 m). ).3,4 Importantly, the range of all droplets, large and small, is extended through their interaction and entrapment within the turbulent gas cloud, compared to the commonly accepted dichotomized droplet model that does not take into account the possibility of a cloud. of hot and humid gas. Furthermore, along the trajectory, droplets of all sizes settle or evaporate at rates that depend not only on their size, but also on the degree of turbulence and velocity of the gas cloud , along with the properties of the environment. (temperature, humidity) and air flow. Droplets that settle along the path can contaminate surfaces, while the rest remain trapped and clumped in the moving cloud. Eventually, the cloud and its payload of droplets lose momentum and coherence, and the remaining droplets within the cloud evaporate, producing debris or droplet nuclei that can remain suspended in the air for hours, following imposed airflow patterns. by ventilation or climate control systems. Evaporation of pathogen-laden droplets in complex biological fluids is poorly understood. The degree and rate of evaporation depend largely on ambient temperature and humidity conditions, but also on the internal dynamics of the turbulent cloud together with the composition of the liquid exhaled by the patient. |
 Gas clouds demonstrate their ability to travel great distances
Gas clouds demonstrate their ability to travel great distances
A 2020 report from China showed that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus particles could be found in ventilation systems in hospital rooms of patients with COVID-19.5.
Finding virus particles in these systems is more consistent with the turbulent model, the gas cloud hypothesis of disease transmission than with the dichotomous model because it explains how viable virus particles can travel long distances from patients. It is unknown if these data have clinical implications regarding COVID-19.
Implications for prevention and precaution
Although no studies have directly evaluated the biophysics of droplets and gas cloud formation for patients infected with the SARS-CoV-2 virus, several properties of exhaled gas cloud and respiratory transmission may apply to this pathogen. If so, this possibility may influence current recommendations aimed at minimizing the risk of disease transmission.
In the World Health Organization’s latest recommendations for COVID-19, healthcare and other personnel are advised to stay between 3 feet (1 m) and 6 feet away from a person who is showing symptoms of illness. , such as coughing and sneezing. The Centers for Disease Control and Prevention recommends a separation of 6 feet (2 m) 7.8.
However, these distances are based on range estimates that have not considered the possible presence of a high momentum cloud that transports the droplets over long distances. Given the dynamic model of turbulent cloud, recommendations for separations of 3 to 6 feet (1-2 m) may underestimate the distance , time scale, and persistence over which the cloud and its pathogenic load travel, thus generating a range of Underestimated potential exposure for a healthcare worker.
| For these and other reasons, wearing appropriate personal protective equipment is critically important for healthcare workers caring for patients who may be infected, even if they are more than 6 feet away from the patient. |
The dynamics of the turbulent gas cloud should influence the design and recommended use of surgical and other masks. These masks can be used for both source control (i.e., reducing spread from an infected person) and protection of the wearer (i.e., preventing spread to an unaffected person).
The protective effectiveness of N95 masks depends on their ability to filter incoming air from aerosolized droplet nuclei. However, these masks are only designed for a certain range of environmental and local conditions and a limited duration of use.9
The effectiveness of the mask as source control depends on the ability of the mask to trap or alter the emission of high momentum gas clouds with their pathogens. Useful load. Peak exhalation velocities can reach up to 33 to 100 feet per second (10-30 m/s), creating a cloud that can span approximately 23 to 27 feet ( 7-8 m ).
Protective and source control masks, as well as other protective equipment, must have the ability to repeatedly resist the type of high- momentum multiphase turbulent gas cloud that can be expelled during a sneeze or cough and exposure to them. Currently used surgical and N95 masks are not tested for these potential respiratory emissions characteristics.
There is a need to understand the biophysics of host-to-host transmission of respiratory diseases that explains the physiology, pathogenesis and epidemiological spread of the disease in the host.
The rapid spread of COVID-19 highlights the need to better understand the dynamics of respiratory disease transmission by better characterizing transmission routes, the role of patient physiology in shaping it, and the best approaches to source control to Potentially improving protection for frontline workers and preventing the disease from spreading to the most vulnerable members of the population.















