After a drop in U.S. reports of sexually transmitted diseases (STDs) early in the COVID-19 pandemic, cases have surged, according to the CDC’s 2020 STD Surveillance Report.
The report noted that the decline in cases was likely due to pandemic-related disruptions in care and several other factors: public health staff diverted from STD work to COVID-19, insurance lapses, shortages of medical supplies. laboratory and telemedicine services that may not have cases recorded in national data. But the short-lived recession was followed by a dramatic resurgence in cases in late 2020.
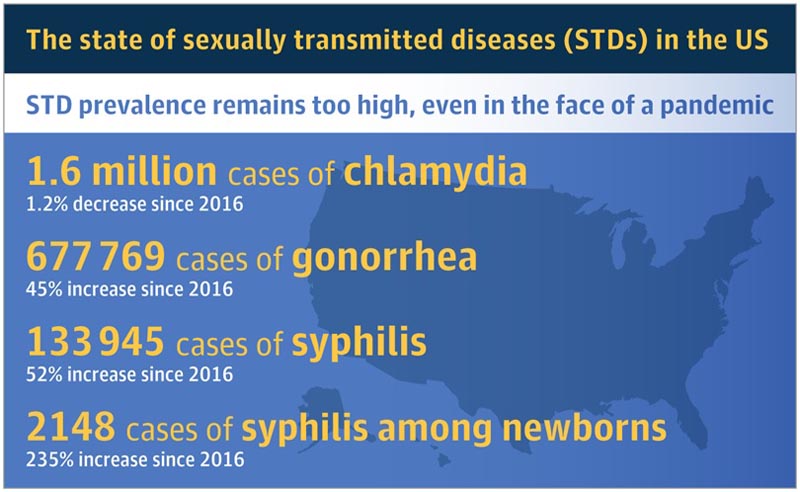
Between 2019 and 2020, reported cases of gonorrhea increased by 10% and cases of primary and secondary syphilis increased by about 7%. Rising syphilis rates also contributed to a 15% increase in congenital syphilis during this period.
In 2020, 2,148 cases of congenital syphilis reported in 47 states, the District of Columbia, and 1 territory included 149 stillbirths or infant deaths. Lack of timely access to prenatal care or failure to screen pregnant women for syphilis contributed to these congenital cases, wrote Leandro Mena, MD, MPH, director of the CDC’s Division of STD Prevention, in a letter to the doctors about the report.
“The COVID-19 pandemic placed enormous pressure on an already overstretched public health infrastructure,” Jonathan Mermin, MD, MPH, director of the National Center for HIV, Viral Hepatitis, STD Prevention, said in a statement. and Tuberculosis from the CDC. “The relentless momentum of the STD epidemic continued even as STD prevention services were disrupted.”
Reported cases of chlamydia, which is often asymptomatic, decreased 13% between 2019 and 2020. The authors of the surveillance report attributed the decline to disruptions in screening rather than a reduction in cases.















